Hemangiomas and Vascular Anomalies
These are abnormal formations originating from vascular structures, most of which are present at birth or appear shortly thereafter. They occur in approximately 1 out of every 1,500 births, with about half of the cases involving the head and neck region.
Vascular anomalies are classified into two main groups:
-
Hemangiomas (infantile hemangiomas)
-
Vascular malformations
Differences Between Hemangiomas and Vascular Malformations
-
Hemangiomas are often first noticed as a small spot by the midwife, nurse, or physician attending the delivery, and they usually begin to grow rapidly within a few weeks after birth.
-
Vascular malformations are mostly present at birth. As the child grows, vascular malformations continue to enlarge proportionally with the child.
-
Hemangiomas gradually change to a darker red color, whereas vascular malformations have a bluish appearance and do not change in color.
HEMANGIOMAS (Infantile Hemangioma)

Figure 1: Infantile hemangiomas located on the nasal dorsum, forehead, lower lip, and sole of the foot.
Hemangiomas are most commonly seen in the head and neck region (65%), followed by the trunk (25%), and then the arms and legs. Hemangiomas may also be located in lymph nodes, spleen, liver, thymus, gastrointestinal system, urinary system, gallbladder, pancreas, adrenal glands, brain, and spinal cord. Hemangiomas are also named according to their postnatal appearance, such as strawberry hemangioma, cherry hemangioma, and port-wine stain.
There are two important developmental phases in hemangiomas:
-
Growth (proliferation) phase
-
Involution (regression) phase
The growth and involution phases occur sequentially after the first year of life. These developmental phases are the most striking characteristics of childhood hemangiomas. Following the rapid growth phase, the hemangioma appears to stop progressing for a period and grows proportionally with the child. This usually occurs between the 6th and 10th months. The first sign of involution is fading of the red color to a pale pink. This change continues until approximately 5 years of age. After involution, mild skin depression (atrophy) may be observed. Clinically, it has been determined that 50% of hemangiomas completely regress before the age of 5, and 70% before the age of 7. The remaining lesions may completely regress by the age of 10–12 or may persist unchanged. However, there are also cases that do not follow this rule and do not enter the involution phase.
PORT-WINE STAIN (PWS)

Figure 2: Port-Wine Stain (PWS)
These are abnormal developments of the intradermal capillary arterial vascular structures. Port-wine stains are present at birth and tend to darken in color as the child grows. They do not regress and retain the same characteristics throughout life. The incidence in newborns is approximately 0.3%. They may sometimes be associated with other malformations, most commonly with Sturge–Weber syndrome. PWS occurs equally in males and females. The skin discoloration, namely the red patch, is usually present at birth; however, it may be overlooked due to the normal redness (erythema) of newborn skin or may become more apparent in cases of anemia. Although PWS can be seen anywhere on the body, in the head and neck region, 45% of cases are limited to one of the three sensory branches of the trigeminal nerve, whereas in 55% of cases the lesion crosses the midline and shows bilateral involvement.
A PWS lesion is flat and well-demarcated and tends to grow proportionally with the child. Its color changes from pale pink to red when the child cries, has a high fever, becomes excited, or is in a warm environment. This pink color darkens as the child enters adolescence and takes on a reddish hue in middle age. With advancing age, the surface of the PWS becomes nodular, giving a cauliflower-like appearance. Pyogenic granuloma commonly develops on PWS lesions, particularly in intraoral lesions. The size, color, and quality of PWS vary from child to child; no two lesions are alike. PWS may also be seen in association with vascular anomalies in other organs and regions as part of syndromic conditions.

Figure 3: Pyogenic Granuloma
Pyogenic granuloma can appear suddenly in all age groups. The lips, oral cavity, tongue, nasal cavity, cheeks, eyelids, hands, and feet are common sites of involvement. Their size rarely exceeds 1 cm. In most cases, there is no history of trauma. The most common clinical finding is bleeding. Ulceration is rarely observed in pyogenic granuloma. Treatment is usually performed with laser therapy.
VENOUS MALFORMATIONS (VM)

Figure 4: Venous Malformation of the Hand and Forearm
Venous malformations are developmental anomalies of venules that are easily recognized by their structural characteristics. Their incidence ranges from 1% to 4% of births.
They are generally seen in association with skeletal anomalies, skin lesions, and capillary and dermovascular lesions. The severity of the malformation may vary from a simple blue discoloration to extensive venous pooling or venous sacs or masses formed by dilated veins. In some cases, these lesions may be accompanied by arterial anomalies.


Figure 5: Venous malformation of the lips and its appearance after laser treatment
Venous malformations are soft lesions that decrease in size when compressed and return to their original form when the pressure is released, and they do not exhibit pulsation (no palpable heartbeat). VM grow proportionally with the child and continue to enlarge unless treated. Venous anomalies may also be located within bone and skeletal muscle without involving the overlying skin. In bones, they are most commonly seen in the jaw, and in muscles, they are frequently found in the muscles of mastication, the thigh, and the leg. Non-congenital VM that are very common in elderly individuals are superficial varicosities, namely varicose veins.

-
Lymphatic Malformations
Lymphatic malformations are anomalies of the lymphatic system that grow slowly along with the child. They are generally found together with venous structures. Therefore, it is more appropriate to use the terms “lymphaticovenous malformation” or “venolymphatic malformation.”
The lymphatic system is located within the skin, subcutaneous tissue, and beneath the fascia. Within the dermis and subdermal layer, the lymphatic system is present at three different plexus levels.
Figure 6: Lymphatic malformations of the face and foot
Lenfatik Malformasyonlarda Tedavi
Surgical Treatment:
-
In well-defined and superficial cases, wide surgical excision is performed.
-
In large cases with ill-defined borders, very careful partial and staged surgical excision is applied.
Laser Treatment:
Since lymphatic malformations (LM) have a fluid-filled (cystic) structure, CO₂ and Nd:YAG lasers are used. However, due to the technical difficulties of CO₂ laser application, there is difficulty in reaching the depth of the lesion.
With the method that I have developed and applied, it is possible to enter the lesion using a fiber-optic extension and affect deeper tissues. In this method, I use a long-pulse Nd:YAG laser. The results are quite satisfactory. With this application, deep intradermal vascular structures and LM lose their volume as a result of excessive thermocoagulation with less blood loss, thereby reducing the size of the LM mass.
After the volume reduction and decrease or disappearance of blood vessels achieved with laser treatment, the remaining fibrotic structures are treated with minor surgical procedures.
TREATMENT OF HEMANGIOMAS
I) Conditions That Require Definitive Treatment
-
Life-threatening localizations:
Cases and syndromes with anatomical localizations that may lead to death in children if left untreated. -
Complications:
Cases with continuous and uncontrollable bleeding, and those causing ulceration and infection. -
Causing functional impairment:
Hemangiomas located on the eyelids and around the eyes that impair vision; lesions located inside or outside the nose and throat that affect eating, drinking, and respiratory functions; and hemangiomas located in and around the ear that impair hearing function.
II) Conditions Requiring Treatment for Social Reasons
Hemangioma cases that do not pose a vital or functional problem are nevertheless known to have negative social effects on the family and the environment. As the child grows, hemangiomas on the face may cause psychological distress due to the child’s own perception when looking in the mirror, as well as insults, teasing, and ridicule from peers, and the curious or pitying looks of relatives, neighbors, and society. As a result of this psychological pressure and harassment, treatment becomes necessary.
TREATMENT OPTIONS FOR HEMANGIOMAS
Treatment criteria for hemangiomas and vascular malformations vary depending on the case and the individual. These can be grouped into two main categories:
1. Non-Invasive Treatments
-
Medical treatments: Use of certain medications (systemic or intralesional corticosteroids), interferon alfa-2a, chemotherapeutic agents, beta-blockers such as Dideral and Timoptic.
-
Sclerosing agents
Invasive Treatments
-
Selective embolization
-
Surgical excision
-
Laser photocoagulation
-
Combined treatment
1. Non-Invasive Treatments
Medical Treatments:
Medical treatment aims to reduce the size of the hemangioma and achieve treatment through the use of medication(s). Currently preferred drugs include corticosteroids, interferon (interferon alfa-2a), chemotherapeutic agents (vincristine, cyclophosphamide, etc.), and beta-blockers (propranolol, timoptol).
Corticosteroid Treatment:
Systemic corticosteroids are generally the first-line agents in medical treatment. Although the success rate ranges between 78% and 89%, their use is limited due to a high recurrence rate of approximately 36% and serious side effects. This treatment should be applied only in selected cases, carefully and with adequate knowledge and experience. It must be performed exclusively by specialist physicians experienced in the treatment of hemangiomas. The exact mechanism by which corticosteroids initiate regression in hemangiomas is still unknown.
Corticosteroid treatment is administered in two ways:
a) Oral (systemic) administration
b) Intralesional (local) administration
Oral Systemic Corticosteroid Treatment:
Prednisolone is administered orally at a dose of 2–3 mg/kg/day for 2–3 weeks. In responsive cases, a response is observed within 7–10 days. The lesion softens, becomes pale, and decreases in size. If no response is obtained, the dose is reduced to 1 mg/kg/day and should be discontinued by the specialist after a certain period. As an alternative approach, after discontinuation of the initial treatment, the dose may be repeated following a rest period of 4–6 weeks. Decisions regarding repeated courses may be made based on age, localization, and the initial response of the lesion. Once the hemangioma enters the involution phase, steroid treatment has no benefit. In lesions in the proliferative phase, a new growth phase may begin after dose reduction. In such cases, treatment at a dose of 1 mg/kg/day for 2–3 weeks should be administered.
The use of high doses is extremely dangerous and requires great caution. Short-term, low-dose prednisolone therapy is associated with relatively few complications. Treated infants may experience decreased appetite and growth retardation. Transient facial edema may develop. There are reports indicating depression of T-cell function and immunological abnormalities in newborns following hydrocortisone administration. Newborns treated with prednisone may be at increased risk for otitis media, pneumonia, and sepsis. Therefore, the lowest effective dose that induces regression in hemangiomas should be administered for the shortest possible duration.
Intralesional Corticosteroid Treatment:
This method was proposed by Mazzola in 1978 and became popular four years later with its use in the periorbital area and eyelids by Kushner. I have achieved very good results with this method and continue to practice it as a plastic surgeon.
Although adrenal suppression has been described in some cases with intralesional corticosteroid (ILS) application, systemic steroid effects are generally not observed. Subcutaneous atrophy (tissue reduction) is observed at the injection site, which is in fact the main therapeutic goal.
In patients unresponsive to corticosteroids, chemotherapeutic agents (vincristine, interferon, cyclophosphamide) may be used as alternatives; however, their efficacy is controversial, and their potential toxicity remains the major concern.
Dideral Kullanımı; Son zamanlarda kullanımı oldukça artan ve sadece infantile hemangioma olgularına değil hemen hemen her hemanjiomlu ve vasküler malformasyonlu hastaya gelişi güzel kullanılan DİDERAL (Propranol) ve TİMOPTİC (timonol) popüler bir hale getirilmiştir.
Dideral 2008 yılında obstrüktif kardiyomyopati nedeni ile oral propranolol tedavisi alan nazal hemanjiomlu bir bebeğin, hemanjiomunun küçüldüğünün tesadüfen fark edilmesiyle, oral propranolol kullanımı da infantil hemanjiom tedavisinde kullanılmaya başlanmıştır. Timoptic (timonol) ise göz içi basıncı düşürmede (glokomda) kullanılan ilaçtır. Her iki ilaç (Propranolol ve Timoptic) Beta bloker olup kalp çalışması ve ritmi üzerine etkilidir. Özellikle 6 aydan küçük bebeklerde hipotansiyon, bronkokonstrüksiyon, (nefes darlığı) bradikardi (nabız düşüklüğü), hipotansiyon, hipoglisemi (şeker düşüklüğü), kardiyak performansta azalma ve erken kardiyak yetmezlik gibi ciddi sorunlara yol açabilen ve hipotansiyona bağlı komplikasyonlara (böbrek yetmezlıği. Beyinin az kanlanmasına bağlı olarak bayılma ve epileptik atak ve konvülsiyonlar ) yol açabilecek ilaçlardır. Bu nedenle bu ilaçlar birçok klinikte çocuk kardiyologları tarafından çeşitli ciddi izlem ve gözlem protokolleriyle yakından izlenmektedir.
Normalde bir yıla kadar beklenildiğinde kendiliğinden gerileyecek olan infantil hemanjiom (İH) olgularına bu ilaç gelişi güzel verilmektedir. Ayrıca bu ilaçların çocuklarda kullanımlarının uzun süredeki komplikasyonlarının neler olduğunu gösteren çalışmalar henüz literature girmemiştir. Bu ilaçların kullanımlarından sonraki dönemlerde (5,10,15 yıl gibi) çocuklarda oluşturdukları yan etki ve sistemik problemlerin neler olacağı da merak konusudur.
*Sklerozan ajanlar: Bu amaçla ergot alkaloidleri, tannik asit, karbonik asit, Fe perklorit, % 95 alkol, kinin hidroklorit, ethamolin, Na tetradesil sülfat, sıcak su, hipertonik salin, hypertonik glikoz, % 5 lik Na morrhuate gibi bir çok madde kullanılmıştır. Alınan sonuçlarda kesin bir hemfikirlilik yoktur.
İnvaziv Tedavi
*Cerrahi Eksizyon: Öncelikli olarak sınırlı kullanımı olup, laser tedavisi sonrasında gerilemeye uğrayarak cerrahiye uygun hale getirilen olgularda kitlenin çıkarılması şeklinde yapılır. Bu sürede genelde okul öncesi 4-5 yaşlarda olmaktadır.
*Selektif embolizasyon: Konjestif kalp yetmezliklerine yol açan K.C ve diğer organ hemangiomlarının, daha önceki kortizon ve lazer tedavilerine cevap vermiyen baş, boyun ve cilt bölgesindeki yüksek kan akımına sahip damarsal lezyonlarda oldukça etkili bir yöntemdir. Bu uygulama radyolog, plastik cerrah ve anestezist işbirliği ile multidisipliner ekip anlayışı içinde tam teşekküllü hastahanelerde uygulanabilen bir yöntemdir. 2 haftalık steroid tedavisine cevapsız kalan baş boyun ve organ lezyonlarında embolizasyona başlanabilir. Bu uygulamanında enfarktüs, felç, Akciğer embolisi ve sepsis (yaygın enfeksiyon) gibi komplikasyonları vardır.
*Laser Fotokoagulasyon: Damarsal Anomaliler için özel olarak üretilmiş Laser cihaz ışınları kandaki hemoglobin (Hb) pigmenti tarafından emilen ışınlardır. Hb tarafından emilen laser ışığı Hb nin aşırı ısınmasına ve Hb nin parçalanmasına neden olur. Böylece Hb nin içinde barındıran damarsal anomaliler fotokoagulasyona yani küçülmeye uğrarlar. Bu amaçla Flashlamp-pumped pulsed dye laser-FPPDL, Argon laser, Potasyum Titaniyl Phosphat – KTP lazer ve Nd YAG lazer olarak kullanılmaktadır.
Laser ile Hemangioma tedavi Endikasyonları:
*Büyüme eğiliminde olan ve diğer tedavilere cevap vermiyen hemangioma ve damarsal lezyonlarda
*Steroid tedavisine yanıt alınamayan ve hızlı büyüme potansiyeline sahip olan hemangioma ve damarsal anomalilerde
*Burun, göz kapağı, kulak, ağız içi ,dudaklar ve solunumu zorlaştıran, boyun üstü ve çevresindeki fonksiyonel, kozmetik ve duyusal alanlardaki damarsal anomalilerde
*Gerilemeye ve küçülmeye uğramış, ancak tam olarak geçmemiş kalıntı halindeki damarsal lezyonlarda.
Lazer Uygulama Yöntemleri
*Lezyon üstü uygulama; Kitlesel yapı oluşturmayan genelde düz ve kabarık olmayan hemanjiom, venöz ve vasküler malformasyonlarda (şarap lekeleri gibi) lezyonun üst kısmına yani deri yüzeyine lazer ışınlarının uygulanması tekniğidir. Her lezyonun kendine has yapı özellikleri olduğundan her hasta kendi içinde değerlendirilir ve lazer dozları ona göre ayarlanarak uygulanır. Uygulamadan önce lezyon üzerine ağrı kesici krem ve pomatlar sürülür. Böylece ağrı duyma hissi azaltılır. Uygulama esnasında da lazer uygulanacak cilt yüzeyine soğuk uygulanması (soğuk hava veya soğuk jel) yapılır. Böylece hastanın rahatsızlık duyması hafifletilir. Küçük çocuklarda ise bu uygulama hafif sedasyon altında yapılır.
*Lezyon içi uygulama: Kitlesel yapı oluşturan ve deri yüzeyinden kabarık olan hemanjiomlar, venöz ve vasküler malformasyonlarda (infaltil hemanjiomalar gibi) lezyon üstü uygulamalar lezyonun iç kısımlarına pek etki edemezler. Daha derin dokuları etkilemek için; özel yaptırılmış fiberoptik uzantı kullanılır. Fiberoptik uzantı vasküler anomalinin içine sokulur. Ve lazer ışığı kitlenin daha derinliklerine ulaştırılır. Böylece lazer ışını kitle içinde daha etkin olur.
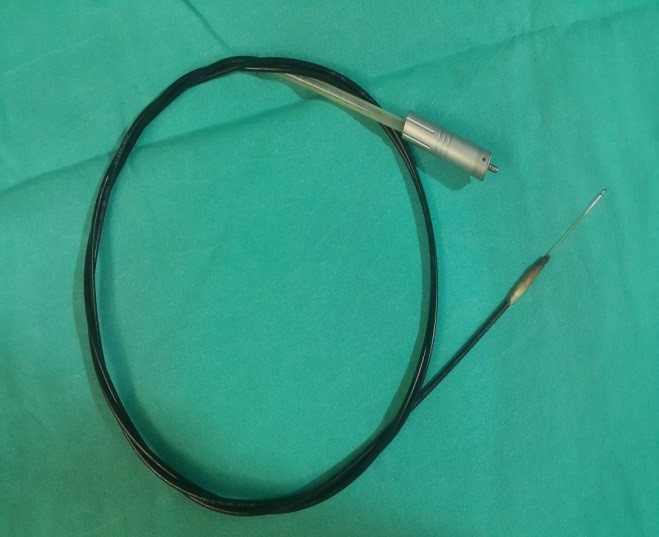
Figure 7: Fiberoptic laser delivery device used for intralesional laser application
-
Intralesional and superficial application
In certain selected hemangiomas, venous, and vascular anomalies, both superficial and intralesional applications are performed simultaneously.
-
Combined treatment

Figure 8: A patient with an upper lip hemangioma treated using a combined method
In patients with aggressive hemangiomas, venous, and vascular malformations that have life-threatening potential, it is possible to apply one or more of the above-mentioned treatment methods together (such as corticosteroids + laser, laser + surgery) in order to reduce the growth rate, eliminate the life-threatening risk, and simultaneously treat the lesion.
VARICOSE VEINS AND THEIR TREATMENT
Veins larger than 3 mm in diameter seen in the legs are called varicose veins. Veins that pump blood back to the heart contain small valves. However, in some individuals—especially pregnant women, overweight individuals, and those who have to stand for long periods—some of these valves become dysfunctional. This causes blood to flow downward directly, leading to dilation of the veins.
Occupations that require prolonged standing in the same position, such as teaching, hairdressing, waiting tables, secretarial work, etc., trigger the formation and rapid progression of varicose veins in the legs.
After vascular deformation, varicose vein disease causes chronic tension and presents with leg swelling, fatigue, and pain. If treatment is delayed, the condition progresses to advanced stages known as secondary diseases. Initially, blue-green dilated capillaries may later turn brown and lead to varicose ulcers in advanced stages.
SYMPTOMS OF VARICOSE VEINS
-
Evening leg pain
-
Unesthetic appearance of the legs and inability to wear skirts
-
Night cramps and pain
-
Swelling around the ankles
-
Non-healing open wounds
TYPES OF VARICOSE VEINS
Varicose veins are classified into four types:
Type I – Telangiectasia:
(Capillary vein rupture) Bright red, superficial veins measuring 0.1–1 mm in diameter, not palpable.
Type II – Venuleectasia:
Blue-purplish, superficial veins measuring 1–3 mm in diameter that feed bright red capillaries, not palpable.
Type III – Reticular veins:
Blue or purplish, deeper-located veins measuring 3–4 mm in diameter, not palpable.
Type IV – Varicose veins:
All visible subcutaneous veins larger than 4 mm. Those seen in the great and small saphenous veins are called truncal, while others are referred to as non-truncal varicose veins.
PREVENTIVE MEASURES
-
Promoting blood circulation with exercises and compression stockings during situations where the calf muscle pump is inactive, such as travel or prolonged sitting
-
Regular exercise (especially swimming, aerobics, running, walking)
-
Elevating the legs above heart level to support venous circulation
-
Avoiding excessive heat (such as Turkish baths and saunas)
-
Using exercise and specially designed compression stockings during pregnancy
-
Avoiding excessive weight, smoking, alcohol consumption, and an irregular lifestyle
-
Avoiding tight clothing that constricts the upper legs
-
Using compression stockings with measured pressure according to your physician’s recommendations
DIAGNOSIS OF VARICOSE VEINS
In patients with varicose veins, color Doppler ultrasound is used to perform a detailed examination of the valves located at the femoral and popliteal junctions, which play a significant role in the development of the disease.
TREATMENT OPTIONS ACCORDING TO THE TYPE OF VARICOSE VEIN
Since most patients have multiple types of varicose veins simultaneously, different treatment methods are combined according to vein type during treatment planning.
Type I–II capillary veins:
Laser therapy, microsclerotherapy
Type III reticular veins:
Sclerotherapy, hook phlebectomy
Type IV varicose veins:
Surgical ligation or removal of veins, hook phlebectomy, foam sclerotherapy, sclerotherapy, radiofrequency ablation, endovenous laser therapy
Laser Treatment of Varicose Veins
Laser technology is based on converting light into thermal energy at the desired tissue depth by utilizing differences in various wavelengths of light. The basis of laser energy use in the treatment of capillary veins lies in the absorption of light by oxygen-carrying red blood cells and its conversion into heat. The resulting heat causes clot formation within the vein, leading to occlusion, shrinkage, and eventual disappearance of the vessel. In our laser center, Type I telangiectasia and Type II venuleectasia lesions are permanently treated using laser applications.
